
Celebrating the Special Moments
CFNR TikTok Videos
“Do it…for me!”
– Lugil Wilaasym hanaa Hyla Denton McQuaid
Harvesting Seaweed “It’s like a family reunion.”
– Litaaladaaw Giybaaw Sharon Bryant
“Don’t be afraid to get your vaccination. It’s so important.”
– Litaaladaaw Giybaaw Sharon Bryant
“Fully Vaccinated…and a Sweet Mullet Just Like Kiefer.”
– Reid Skeleton Morven
“Just Another Day At The Office”
– Kuuk’ Iiwaans Kiefer Collison
Looking forward to being at all the events coming our way!
– Kuuk’ Iiwaans Kiefer Collison
“Fully Vaccinated, and a Sweet Mullet”
– Kuuk’ Iiwaans Kiefer Collison
“Haida Gwaii…At Last!”
– Kuuk’ Iiwaans Kiefer Collison
“‘Kiefer Day’ in Gitlaxt’aamiks”
– Kuuk’ Iiwaans Kiefer Collison
TikTok #1
Hlkuu Weex Wanda Good
TikTok #2
Hlkuu Weex Wanda Good
Vaccine TikTok #1
Lugil Wilaasym hanaa Hyla Denton McQuaid
Vaccine TikTok #2
Lugil Wilaasym hanaa Hyla Denton McQuaid
Vaccine TikTok #1
Wiigyaxs Ravyn Good
Vaccine TikTok #2
Wiigyaxs Ravyn Good
We’re Here For You (Video)
Here’s what we at CFNR are doing to keep healthy during these tough times
Wash Your Hands..! (Video)
Kief’n You Safe (Video)
Kiefer Collison has a few tips and reminders for us about how to keep us and our loved ones safe.
CFNR “Journeys” Radio Program
“This means Freedom”
– Litaaladaaw Giybaaw Sharon Bryant
“I have a responsibility to my community.”
– Hlkuu Weex Wanda-Good
Kuuk’ Iiwaans Kiefer Collison and his thoughts on Vaccinating
– Kuuk’ Iiwaans Kiefer Collison
Kiefer sat down and chatted with Char about his thought process about getting the vaccine.
If you are struggling and need additional help:
www.canada.ca/en/public-health/services/mental-health-services/mental-health-get-help
COVID Resources and Information
The Vaccine
Vaccines FAQ
There has been a lot in the news about vaccines and we know it can be confusing, overwhelming and exciting. We want to help you understand them and then empower you to decide if getting a vaccine is right for you, for your family and for your community. Below you’ll find answers to the most commonly asked questions about the vaccines.
https://bc.thrive.health/covid19app/vaccines/faq
Was the development of the COVID-19 vaccines rushed? Do we really know the vaccines are safe?
mRNA vaccines have been in development for many years. All COVID-19 vaccines approved by Health Canada are safe. The medical and scientific community is confident in the vaccines’ safety because of the track record of Canada’s (and BC’s) vaccine approval and safety monitoring system. Over 19 million Canadians have been fully and safely vaccinated, most with an mRNA vaccine. Learn more about how BC will monitor vaccine uptake, safety, and effectiveness.
Does the COVID-19 vaccine still work if there is a shorter or longer time between doses? How do we know that different intervals are okay?
The BC government recommends you get your second dose as early as four weeks after your first dose, depending on what is happening in your community.
If you live or work in a community experiencing a COVID-19 outbreak, get your second dose as soon as you can (as soon as four weeks). If you do not live or work in one of these areas, getting your second dose six to eight weeks after your first dose may provide stronger protection.
Generally, vaccine manufacturing companies and national vaccine advisory bodies specify the shortest acceptable timeframe (minimum interval) between vaccine doses but do not specify maximum intervals. For many vaccines, a longer interval to the booster dose results in higher antibody levels. High antibody levels are associated with longer protection time.
The goal is to complete the vaccine schedule and get the total recommended number of doses.
Your COVID-19 Vaccination
Your COVID-19 Vaccine
- COVID-19 vaccines are safe and effective.
- Everyone 5 years and older is now eligible to get a free COVID-19 vaccination.
- Learn about the different vaccines available.
- Search vaccines.gov, text your zip code to 438829, or call 1-800-232-0233 to find COVID-19 vaccine locations near you.

If you are fully vaccinated, you can resume many activities that you did prior to the pandemic. Learn more about what you can do when you have been fully vaccinated.


Before You Get the Vaccine
- Should I get vaccinated if I’ve had COVID-19?
- Should I take medications before getting the vaccine?
- Can I have other medical procedures before or after the vaccine?
Vaccine Information for Specific Groups of People
- What if I’m at risk for severe illness?
- Can my child get vaccinated?
- What if I’m pregnant or breastfeeding?

When You Get the Vaccine
- What are the possible side effects?
- Do I need a booster shot?
- Register for v-safe

When You’ve Been Fully Vaccinated
- How long after my shot am I fully vaccinated?
- What things can I do after I’m fully vaccinated?
- Do I need to wear a mask after I’m fully vaccinated?
Other Questions? See Frequently Asked Questions
COVID-19 Immunization Plan
Last updated: Nov 19, 2021 3:11 PM
All COVID-19 vaccines in Canada are effective and safe. The best vaccine is the one available to you.
B.C.’s COVID-19 Immunization Plan is designed to save lives and stop the spread of COVID-19. The next phase of the plan is focused on sustained protection for everyone.
Dose 3 for people who are moderately to severely immunocompromised
- People with moderately to severely compromised immune systems will receive a third dose of vaccine. Review dose 3 criteria
Booster dose
- Everyone 18 and older will be invited to get a booster dose of the COVID-19 vaccine. Learn more about boosters
Vaccines for children 5 to 11 are coming soon.
- Parents can register their child now to get ready
Not vaccinated yet? If you’re over 12 and haven’t received your first dose, register today.
Priority Populations
Last updated: Nov 19, 2021 3:11 PM
Most people with COVID-19 recover; however, some people have an increased chance of developing severe illness or complications from COVID-19 including older people and those with chronic health conditions. Other patients may have questions about how their health may be impacted by COVID-19.
Here you can find information for:
- People with chronic health conditions
- Children with immune suppression
- (PDF) Children with medical complexity
- HIV and COVID-19
- Tuberculosis and COVID-19
- People living with kidney disease
- Patients receiving cancer treatment
- People who may be or are experiencing violence
- People who are unsheltered
- People who use substances
- People with disabilities
Information about visiting a pharmacy and accessing medication:
(PDF) COVID-19 Language guide: Guidelines for inclusive language and digital content.
BC & The Vaccine Card
BC Vaccine Card Information
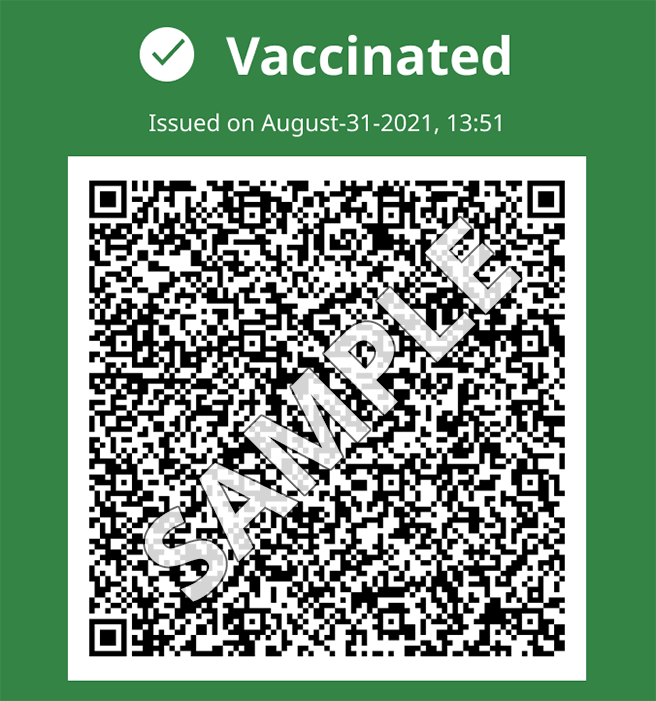
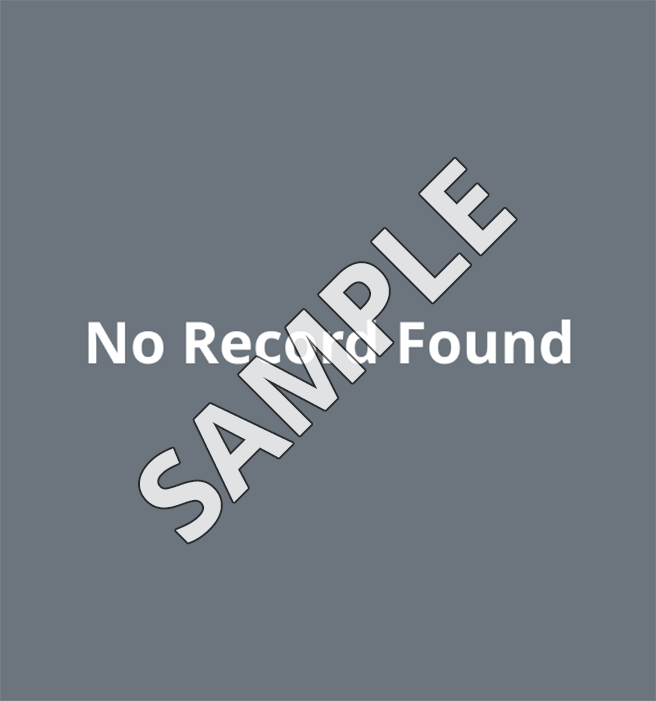
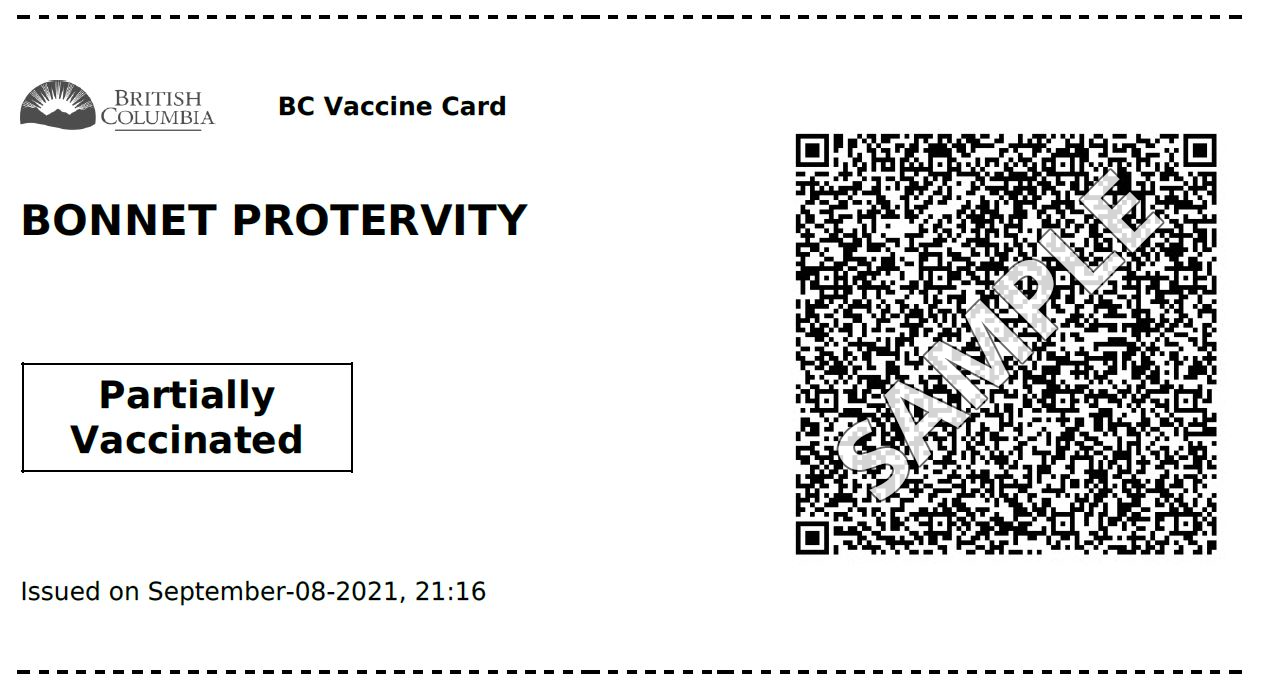
What the BC Vaccine Card looks like
You can save the digital version to your phone or tablet or print a paper copy to carry in your wallet. Both options are accepted everywhere.
Digital card
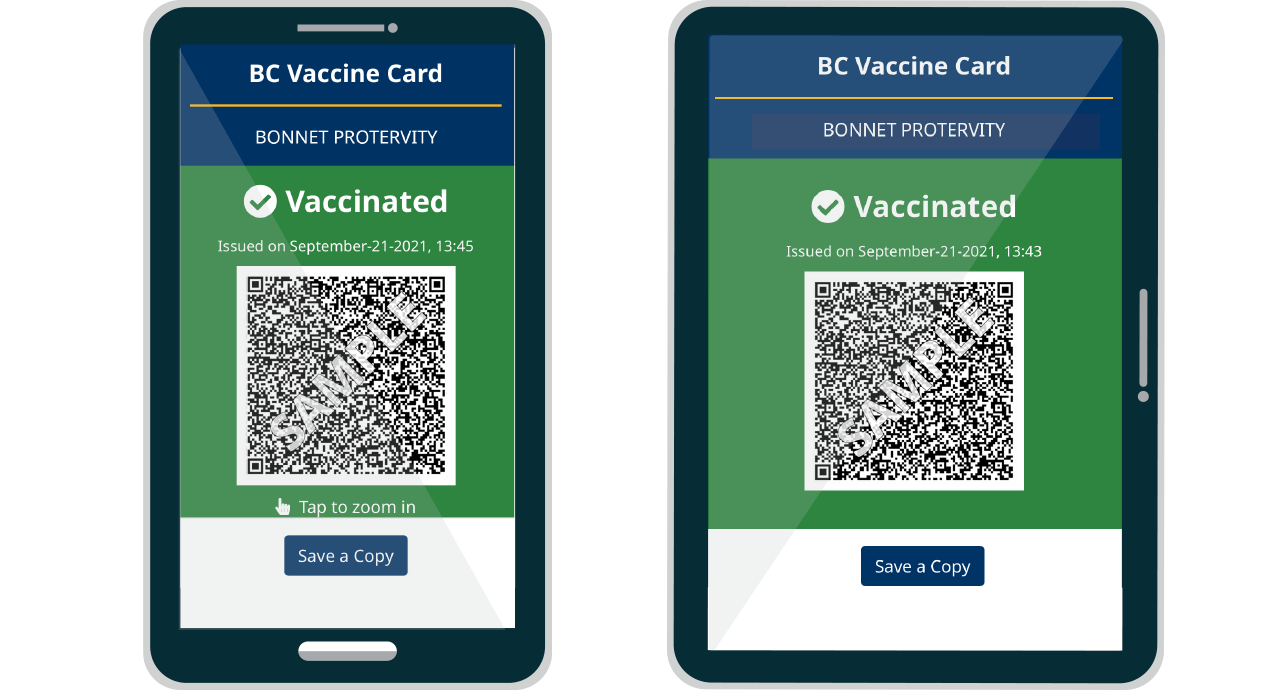
Paper card
Your Card, Going Out & Privacy
Places proof of vaccination is required for entry
This content is a summary of the PHO order – Food and Liquor Serving Premises (PDF, 402KB) and PHO order – Gatherings and Events (PDF, 483KB) documents. It is not legal advice and does not provide an interpretation of the law. In the event of any conflict or difference between this webpage and the order, the order is correct and legal and must be followed.
By order of the Provincial Health Officer (PHO), proof of full vaccination is required to access some events, services and businesses. The requirement is in place until January 31, 2022 and could be extended.
The requirement applies to all people born in 2009 or earlier (12+) and covers:
- Indoor organized events with more than 50 people
- For example, weddings, funeral receptions (outside of a funeral home), organized parties, conferences, trade fairs and workshops
- Indoor concerts, theatre, dance and symphony events with more than 50 people
- Licensed restaurants and cafes and restaurants and cafes that offer table service (indoor and patio dining)
- Includes liquor tasting rooms in wineries, breweries or distilleries
- Pubs, bars and lounges (indoor and patio dining)
- Nightclubs, casinos and movie theatres
- Post-secondary student housing
- Indoor organized group recreational classes and activities with more than 50 people
- For example, pottery studios, art classes or choir rehearsals
- Indoor ticketed sporting events with more than 50 people
- Indoor adult group and team sports for people 22 years old or older
- Spectators at indoor youth sporting events
- Unpaid supervisors, coaches and assistants of sports and group activities for people 21 years or younger
- Indoor skating rinks
- Businesses offering indoor exercise/fitness
- Gyms, exercise and dance facilities or studios
- Includes these activities happening in recreation facilities
Examples of places that don’t require proof of vaccination
You don’t have to show proof of vaccination at places like:
- Grocery stores, liquor stores and pharmacies
- Unlicensed restaurants that don’t offer table service
- For example, fast food, coffee shops, food courts, food trucks and takeout
- Tasting rooms without seating attached to wineries, breweries or distilleries
- Local public transportation (BC Transit, TransLink, BC Ferries)
- Salons, hairdressers and barbers
- Hotels, resorts, cabins and campsites
- Does not include settings or events covered by the PHO order, for example, a licensed hotel restaurant, wedding reception or conference
- Does not include exercise/fitness facilities for guests
- Swimming pools and activities at pools
- Banks and credit unions
- Retail and clothing stores
- Public libraries, museums and art galleries
- Does not include events hosted in these venues
- Food banks and shelters
Privacy and your BC Vaccine Card
Your QR code is not connected to other health records. B.C. uses the SMART Health Card QR code format, a requirement of the federal government.
Don’t share your QR code on social media. This is a personal document.
Every card has a unique QR code
Each QR code contains:
- Full name pulled from your B.C. driver’s licence or BC Services Card
- Date of birth
- Dates of vaccination
- Type of vaccine and dose lot numbers
- Clinic location of each dose
Privacy with businesses
In B.C., businesses that scan your QR code are required to use the BC Vaccine Card Verifier app. The app only displays:
- Your name
- If you are partially or fully vaccinated
Businesses aren’t allowed to keep a copy of this information without your consent.
What your vaccine card shows
Partially vaccinated
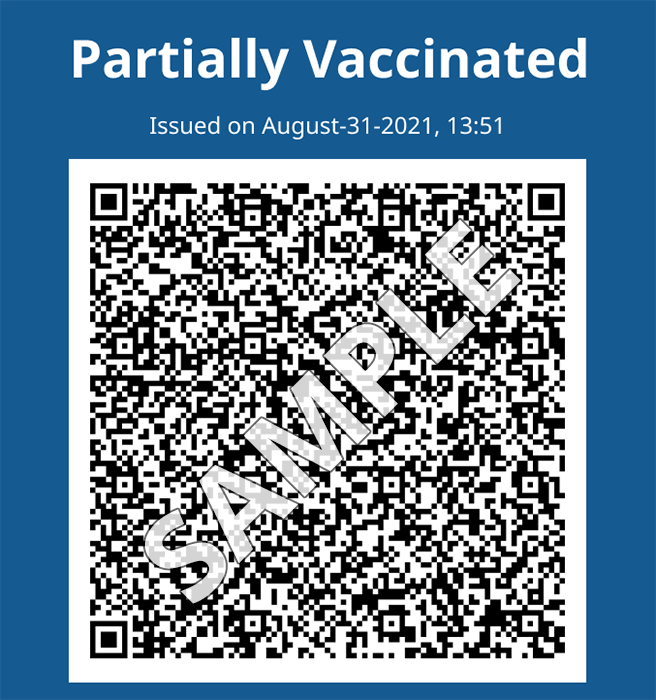
- One dose of vaccine
- Doesn’t meet the proof requirement
Checking ID
Events, businesses and services will ask to see your BC Vaccine Card and a piece of valid government photo ID, for example:
- B.C. driver’s licence or BC Services Card
- You can use your interim driver’s licence, usually printed on yellow paper
- Passport
- Photo ID issued by another province or territory
If your name is wrong on your BC Vaccine Card
If you have legally changed your name, but your vaccine card still shows your old name, you should:
- Try re-downloading your vaccine card from Health Gateway
- Call 1-833-838-2323 to have your legal name manually updated on your vaccine card
If your name is wrong on your driver’s licence or BC Services Card
If the name on your B.C. driver’s licence or BC Services Card does not reflect your current name, you should update your ID.
For example, your current name may be different if you’ve recently been married, divorced or legally changed your name.
Learn more about what you can do if you’re not able to update your ID.
Families and caregivers
You can share copies of your vaccine card with your family and loved ones. We recommend emailing copies to family members or printing multiple copies.
Parents should carry a copy of their child’s vaccine card with them. You are allowed to have multiple copies.
Students and youth
Post-secondary students
Proof of vaccination is also required for some on-campus housing.
Out-of-province students
You can use your provincial/territorial or international proof of vaccination. If you want, you can get a BC Vaccine Card. There are 2 steps to get a card:
- Get a B.C. Personal Health Number (PHN). Call 1-833-838-2323 and one will be created for you
- Upload your out-of-province proof of vaccination to our online form
Youth aged 12 to 18
Youth aged 12 to 18 can carry their own BC Vaccine Card, or have a trusted adult carry it for them.
Youth are not required to show valid government photo ID.
Canadian and US Armed Forces
Members of the Canadian and US Armed Forces don’t need to get a BC Vaccine Card.
Canadian Armed Forces can use their National Defence Canada COVID-19 vaccine record or card and National Defence ID card.
Visiting US Armed Forces can use their US Military proof of vaccination and US Military ID card.
People who don’t have B.C. ID
People who don’t have a B.C. ID are also required to show proof of vaccination. You might not have B.C. identification if:
- You’re visiting from another place
- You just moved here
People from other provinces or territories
People from other Canadian provinces or territories must show:
- Provincial/territorial vaccine record or federal proof of vaccination
- Valid government photo ID
I need help
Federal Vaccination Proof and Travel
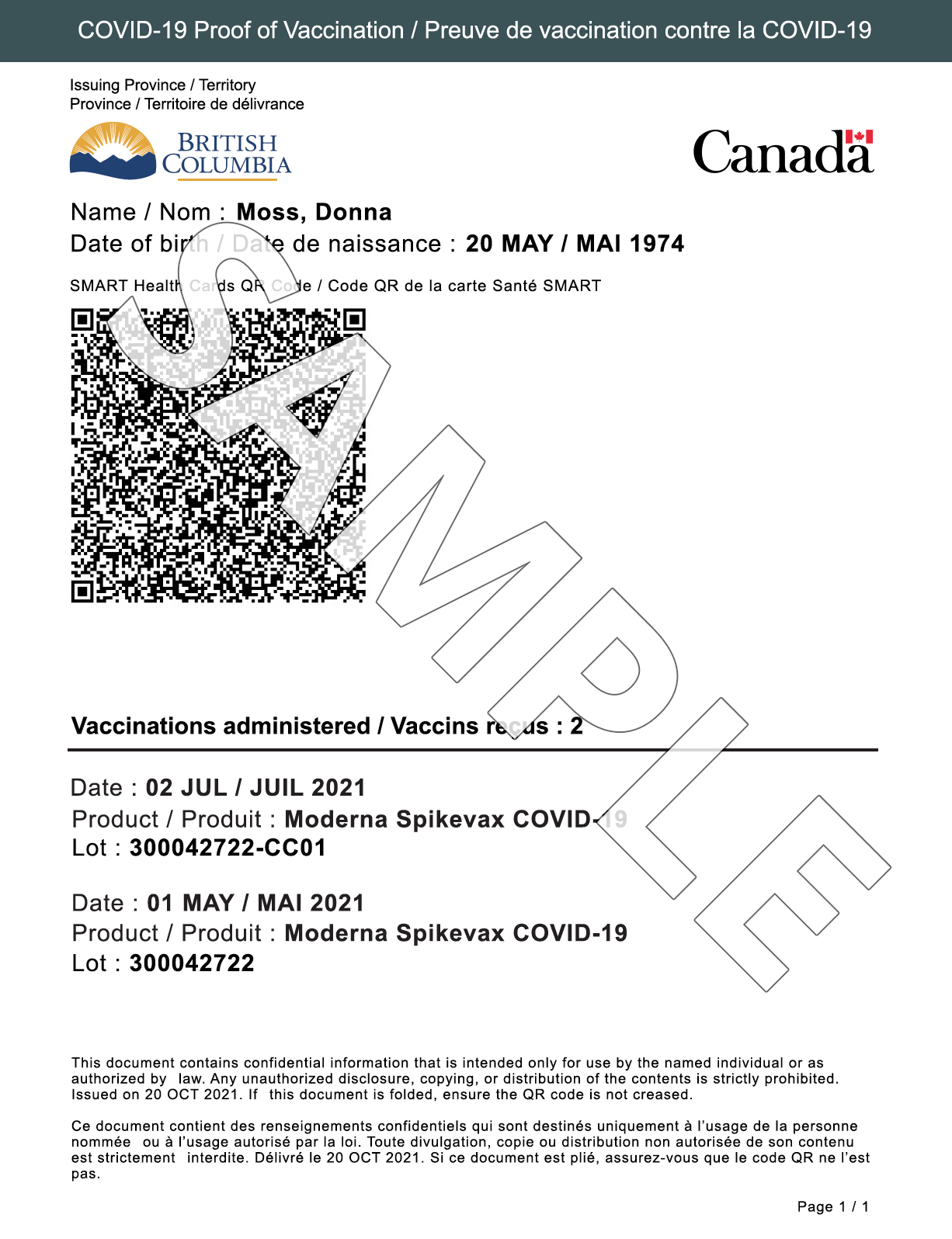
Federal COVID-19 proof of vaccination for travel
The Government of Canada has created a federal COVID-19 proof of vaccination document for travel. It’s recommended you use the document for travel within Canada and internationally.
What the federal COVID-19 proof of vaccination looks like
The federal COVID-19 proof of vaccination document has the Government of Canada flag and a QR code that contains your COVID-19 vaccination history.
How to get the federal COVID-19 proof of vaccination
People who live in B.C. have 3 options to get Canada’s COVID-19 proof of vaccination for travel, the same way you got your BC Vaccine Card. It’s free to get. If someone is asking you to pay for the document, it’s a scam.
Travelling internationally
Many international destinations may accept Canada’s COVID-19 proof of vaccination. Each country makes the final decision on what they accept as proof of vaccination.
When you return to Canada, you must use ArriveCAN to submit your travel and health details in the 72 hours before your arrival back in the country.
Travel and COVID-19

If you’re travelling within Canada or leaving the country, make a plan to show proof of vaccination.
Last updated: November 10, 2021
On this page:
- Federal requirements for travel within Canada
- Federal COVID-19 proof of vaccination for travel
- Travelling internationally
Federal requirements for travel within Canada
The Government of Canada requires all travellers 12 years and 4 months of age and older to be fully vaccinated and show proof of vaccination to use federally regulated methods of travel:
- Departing from any Canadian airport
- Travelling on VIA Rail and Rocky Mountaineer trains
- Staying on a non-essential passenger vessel for more than 24 hours (like a cruise ship)
- BC Ferries does not require proof of vaccination
Note: For travel within Canada, you’re considered fully vaccinated 14 days after you get your second dose of vaccine.
During the transition period to November 30, 2021, anyone who is partially vaccinated can travel if they show a negative COVID-19 molecular test from within 72 hours prior to departure.
Federal COVID-19 proof of vaccination for travel
The Government of Canada has created a federal COVID-19 proof of vaccination document for travel. It’s recommended you use the document for travel within Canada and internationally.
What the federal COVID-19 proof of vaccination looks like
The federal COVID-19 proof of vaccination document has the Government of Canada flag and a QR code that contains your COVID-19 vaccination history.
How to get the federal COVID-19 proof of vaccination
People who live in B.C. have 3 options to get Canada’s COVID-19 proof of vaccination for travel, the same way you got your BC Vaccine Card. It’s free to get. If someone is asking you to pay for the document, it’s a scam.
Travelling internationally
Many international destinations may accept Canada’s COVID-19 proof of vaccination. Each country makes the final decision on what they accept as proof of vaccination.
When you return to Canada, you must use ArriveCAN to submit your travel and health details in the 72 hours before your arrival back in the country.
What to do if you or a loved one gets COVID
Caring for Someone Sick at Home
Advice for caregivers in non-healthcare settings
If you are caring for someone with COVID-19 at home or in a non-healthcare setting, follow this advice to protect yourself and others. Learn what to do when someone has symptoms of COVID-19 or when someone has been diagnosed with the virus. This information also should be followed when caring for people who have tested positive but are not showing symptoms.
*Note: Older adults and people of any age with serious underlying medical conditions are at higher risk for developing more severe illness from COVID-19. People at higher risk of severe illness should call their doctor as soon as symptoms start.
Provide support

Make sure the person who is sick drinks a lot of fluids and rests
- Help the person who is sick follow their doctor’s instructions for care and medicine.
- For most people, symptoms last a few days, and people usually feel better after a week.
- See if over-the-counter medicines for fever help the person feel better.
- Make sure the person who is sick drinks a lot of fluids and rests.
- Help them with grocery shopping, filling prescriptions, and getting other items they may need. Consider having the items delivered through a delivery service, if possible.
- Take care of their pet(s), and limit contact between the person who is sick and their pet(s) when possible.
- Have their doctor’s phone number on hand.
- Use CDC’s self-checker tool to help you make decisions about seeking appropriate medical care.
- Call their doctor if the person keeps getting sicker. For medical emergencies, call 911 and tell the dispatcher that the person has or might have COVID-19.
Look for emergency warning signs* for COVID-19. If someone is showing any of these signs, seek emergency medical care immediately:
- Trouble breathing
- Persistent pain or pressure in the chest
- New confusion
- Inability to wake or stay awake
- Pale, gray, or blue-colored skin, lips, or nail beds, depending on skin tone
*This list is not all possible symptoms. Please call your medical provider for any other symptoms that are severe or concerning to you.
Call 911 or call ahead to your local emergency facility: Notify the operator that you are seeking care for someone who has or may have COVID-19.
Protect yourself

Keep a separate bedroom and bathroom for a person who is sick
COVID-19 spreads between people who are in close contact (within about 6 feet) through respiratory droplets, created when someone talks, coughs or sneezes. Staying away from others helps stop the spread of COVID-19.
The caregiver, when possible, should not be someone who is at higher risk for severe illness from COVID-19.
The person who is sick should isolate
The sick person should separate themselves from others in the home. Learn when and how to isolate.
- If possible, have the person who is sick use a separate bedroom and bathroom. If possible, have the person who is sick stay in their own “sick room” or area and away from others. Try to stay at least 6 feet away from the sick person.
- Shared space: If you have to share space, make sure the room has good air flow.
- Open the window to increase air circulation.
- Improving ventilation helps remove respiratory droplets from the air.
- Avoid having visitors. Avoid having any unnecessary visitors, especially visits by people who are at higher risk for severe illness.
Caregivers should quarantine
Caregivers and anyone who has been in close contact with someone who has COVID-19 should stay home, except in limited circumstances. Learn when and how to quarantine.
Deciding when it is safe to be around others is different for different situations. Find out when someone who is sick can safely end home isolation.
- Stay separated: The person who is sick should eat (or be fed) in their room, if possible.
- Wash dishes and utensils using gloves and hot water: Handle any dishes, cups/glasses, or silverware used by the person who is sick with gloves. Wash them with soap and hot water or in a dishwasher.
- Clean hands after taking off gloves or handling used items.
- If you are not fully vaccinated and aged 2 or older, you should wear a mask in indoor public places.
- In general, you do not need to wear a mask in outdoor settings.
- In areas with high numbers of COVID-19 cases, consider wearing a mask in crowded outdoor settings and for activities with close contact with others who are not fully vaccinated.
- If you are fully vaccinated and have a condition or are taking medications that weaken your immune system, you may need to keep taking steps to protect yourself, like wearing a mask. Talk to your healthcare provider about steps you can take to manage your health and risks.
- If you are fully vaccinated, see When You’ve Been Fully Vaccinated.
The person who is sick
- The person who is sick should wear a mask when they are around other people at home and out (including before they enter a doctor’s office).
- The mask helps prevent a person who is sick from spreading the virus to others. It keeps respiratory droplets contained and from reaching other people.
- Masks should not be placed on young children under age 2, anyone who has trouble breathing, or is not able to remove the covering without help.
Caregiver
- Put on a mask and ask the sick person to put on a mask before entering the room.
- Wear gloves when you touch or have contact with the sick person’s blood, stool, or body fluids, such as saliva, mucus, vomit, and urine. Throw out gloves into a lined trash can and wash your hands right away.
- Practice everyday preventive actions to keep from getting sick: wash your hands often; avoid touching your eyes, nose, and mouth; and frequently clean and disinfect surfaces.
Note: During the COVID-19 pandemic, medical grade masks are reserved for healthcare workers and some first responders.
- Wash hands: Wash your hands often with soap and water for at least 20 seconds. Tell everyone in the home to do the same, especially after being near the person who is sick.
- Hand sanitizer: If soap and water are not readily available, use a hand sanitizer that contains at least 60% alcohol. Cover all surfaces of your hands and rub them together until they feel dry.
- Hands off: Avoid touching your eyes, nose, and mouth with unwashed hands.
- Learn more about handwashing.
When and how to clean surfaces and objects
Cleaning with a household cleaner that contains soap or detergent reduces the amount of germs on surfaces and objects and decreases risk of infection from surfaces. In most situations, cleaning alone removes most virus particles on surfaces.
- Clean high-touch surfaces and objects regularly (for example, daily or after each use) and after you have visitors in your home.
- Focus on high-touch surfaces and objects (doorknobs, tables, handles, light switches, phones, remote controls, and countertops).
- Clean other surfaces in your home when they are visibly dirty or as needed. Clean them more frequently if people in your household are more likely to get very sick from COVID-19. Disinfect if certain conditions apply.
- Clean surfaces using a product suitable for each surface, following instructions on the product label.
When Someone Is Sick
If someone in your home is sick or someone who has COVID-19 has been in your home in the last 24 hours, clean and disinfect your home. Disinfecting removes germs and reduces their spread.
For more information on cleaning and disinfecting safely, see Cleaning and Disinfecting Your Home.
- Caregivers should stay home and monitor their health for COVID-19 symptoms while caring for the person who is sick.
- Symptoms include fever, cough, and shortness of breath but other symptoms may be present as well. Trouble breathing is a more serious warning sign that you need medical attention.
- Caregivers should continue to stay home after care is complete. Caregivers can leave their home 14 days after their last close contact with the person who is sick (based on the time it takes to develop illness), or 14 days after the person who is sick meets the criteria to end home isolation.
- The best way to protect yourself and others is to stay home for 14 days if you think you’ve been exposed to someone who has COVID-19. Check your local health department’s website for information about options in your area to possibly shorten this quarantine period.
- Use CDC’s self-checker tool to help you make decisions about seeking appropriate medical care.
- If you are having trouble breathing, call 911.
- Call your doctor or emergency room and tell them your symptoms before going in. They will tell you what to do.
Self-Isolation and Self-Monitoring
When you self-monitor, check yourself for symptoms of COVID-19 and get tested right away if you think you may be sick.
When you self-isolate, stay home and keep away from others to help stop the spread of COVID-19.
Last updated: August 23, 2021
- If you have been exposed to someone with COVID-19, you will need to self-monitor for 14 days.
- Some close contacts may also need to self-isolate for part of that time. For example, if you are not fully vaccinated, you may need to self-isolate for 10 of the 14 days.
- Follow the directions provided to you by Public Health.
- Being sufficiently protected by vaccination means you have received all the recommended vaccine doses and had time to develop a better immune response after receiving the last dose.
Quarantine and Isolation
- You quarantine when you might have been exposed to the virus.
- You isolate when you have been infected with the virus, even if you don’t have symptoms.
For detailed CDC recommendations for public health agencies on the duration of quarantine, see Science Brief: Options to Reduce Quarantine.
Quarantine
Quarantine if you have been in close contact (within 6 feet of someone for a cumulative total of 15 minutes or more over a 24-hour period) with someone who has COVID-19, unless you have been fully vaccinated. People who are fully vaccinated do NOT need to quarantine after contact with someone who had COVID-19 unless they have symptoms. However, fully vaccinated people should get tested 5-7 days after their exposure, even if they don’t have symptoms and wear a mask indoors in public for 14 days following exposure or until their test result is negative.
What to do
- Stay home for 14 days after your last contact with a person who has COVID-19.
- Watch for fever (100.4◦F), cough, shortness of breath, or other symptoms of COVID-19.
- If possible, stay away from people you live with, especially people who are at higher risk for getting very sick from COVID-19.
After quarantine
- Watch for symptoms until 14 days after exposure.
- If you have symptoms, immediately self-isolate and contact your local public health authority or healthcare provider.
You may be able to shorten your quarantine
Your local public health authorities make the final decisions about how long quarantine should last, based on local conditions and needs. Follow the recommendations of your local public health department if you need to quarantine. Options they will consider include stopping quarantine
- After day 10 without testing
- After day 7 after receiving a negative test result (test must occur on day 5 or later)
Isolation
Isolation is used to separate people infected with COVID-19 from those who are not infected.
People who are in isolation should stay home until it’s safe for them to be around others. At home, anyone sick or infected should separate from others, stay in a specific “sick room” or area, and use a separate bathroom (if available).
What to do
- Monitor your symptoms. If you have an emergency warning sign (including trouble breathing), seek emergency medical care immediately.
- Stay in a separate room from other household members, if possible.
- Use a separate bathroom, if possible.
- Avoid contact with other members of the household and pets.
- Don’t share personal household items, like cups, towels, and utensils.
- Wear a mask when around other people if able.
Learn more about what to do if you are sick and how to notify your contacts.
When You Can be Around Others After You Had or Likely Had COVID-19
Most people do not require testing to decide when they can be around others; however, if your healthcare provider recommends testing, they will let you know when you can resume being around others based on your test results.
For Anyone Who Has Been Around a Person with COVID-19
Anyone who has had close contact with someone with COVID-19 should quarantine for 14 days after their last exposure to that person, except if they meet the following conditions:
Someone who has been fully vaccinated and shows no symptoms of COVID-19 does not need to quarantine. However, fully vaccinated close contacts should:
- Wear a mask indoors in public for 14 days following exposure or until a negative test result.
- Get tested 5-7 days after close contact with someone with suspected or confirmed COVID-19.
- Get tested and isolate immediately if experiencing COVID-19 symptoms.
Someone who tested positive for COVID-19 with a viral test within the previous 90 days and has subsequently recovered and remains without COVID-19 symptoms does not need to quarantine. However, close contacts with prior COVID-19 infection in the previous 90 days should:
- Wear a mask indoors in public for 14 days after exposure.
- Monitor for COVID-19 symptoms and isolate immediately if symptoms develop.
- Consult with a healthcare professional for testing recommendations if new symptoms develop.
I think or know I had COVID-19, and I had symptoms
You can be around others after:
- 10 days since symptoms first appeared and
- 24 hours with no fever without the use of fever-reducing medications and
- Other symptoms of COVID-19 are improving*
*Loss of taste and smell may persist for weeks or months after recovery and need not delay the end of isolation
Note that these recommendations do not apply to people with severe COVID-19 or with weakened immune systems (immunocompromised).
I tested positive for COVID-19 but had no symptoms
If you continue to have no symptoms, you can be with others after 10 days have passed since you had a positive viral test for COVID-19.
If you develop symptoms after testing positive, follow the guidance above for “I think or know I had COVID-19, and I had symptoms.”
I was severely ill with COVID-19 or have a weakened immune system (immunocompromised) caused by a health condition or medication.
People who are severely ill with COVID-19 might need to stay home longer than 10 days and up to 20 days after symptoms first appeared. People with weakened immune systems may require testing to determine when they can be around others. Talk to your healthcare provider for more information. Your healthcare provider will let you know if you can resume being around other people based on the results of your testing.
People who are immunocompromised should be counseled about the potential for reduced immune responses to COVID-19 vaccines and the need to continue to follow current prevention measures (including wearing a mask, staying 6 feet apart from others they don’t live with, and avoiding crowds and poorly ventilated indoor spaces) to protect themselves against COVID-19 until advised otherwise by their healthcare provider. Close contacts of immunocompromised people should also be encouraged to be vaccinated against COVID-19 to help protect these people.
For Healthcare Professionals
If you are a healthcare professional who thinks or knows you had COVID-19, you should follow the same recommendations listed above for when you can resume being around others outside the workplace. When you can return to work depends on different factors and situations. For information on when you can return to work, see the following:
Criteria for Return to Work for Healthcare Personnel with SARS-CoV-2 Infection (Interim Guidance)
If you have or think you might have COVID-19, it is important to stay home and away from others. When you can be around others depends on different factors for different situations.
If you have or think you might have COVID-19, it is important to stay home and away from others. When you can be around others depends on different factors for different situations.
How do people living together manage quarantine when they cannot be separated from the person with COVID-19?
It is very important for people with COVID-19 to remain apart from other people if possible, even if they are living together. If separation of the person with COVID-19 from others in the home is not possible, the other members of the household will have ongoing exposure, meaning they will be repeatedly exposed until that person is no longer able to spread the virus to other people.
People with COVID-19 can spread the virus to other people for 10 days after they develop symptoms, or 10 days from the date of their positive test if they do not have symptoms. The person with COVID-19 and all members of the household should wear a well-fitted mask and consistently, inside the home. If possible, one member of the household should care for the person with COVID-19 to limit the number of people in the household that are in close contact with the infected person. Take steps to protect yourself and others to reduce transmission in the home. Quarantine is a strategy to prevent transmission of COVID-19. It ensures that unvaccinated or not fully vaccinated people who have been in close contact with someone with COVID-19 stay apart from others. You quarantine when you have been exposed to the virus that causes COVID-19 and are unvaccinated or not fully vaccinated. Isolation is a strategy to prevent transmission of COVID-19 by separating people with COVID-19 from those who are not infected. You isolate when you have symptoms of COVID-19 or are infected with the virus that causes COVID-19, even if you don’t have symptoms.
Public health recommendations for testing and quarantine of close contacts with ongoing exposure depend on vaccination status.
What are the public health recommendations for close contacts who have ongoing exposure to COVID-19?
Close contacts with ongoing exposure who are unvaccinated or not fully vaccinated
People who are unvaccinated or not fully vaccinated and have ongoing exposure to COVID-19 should
- Get tested immediately when they are identified as a close contact.
- Begin quarantine immediately and continue to quarantine throughout the isolation period of the person with COVID-19.
- Continue to quarantine for an additional 14 days starting the day after the end of isolation for the person with COVID-19.
- Get tested again 5-7 days after the end of isolation of the infected household member.
- Wear a mask when in contact with the person with COVID-19 throughout the person’s isolation period.
- Wear a mask when in contact with other people in the home until quarantine ends.
- Isolate immediately if they develop symptoms of COVID-19 or test positive.
Close contacts with ongoing exposure who are fully vaccinated
People who are fully vaccinated and have ongoing exposure to COVID-19 should
- Get tested 5-7 days after their first exposure. A person with COVID-19 is considered infectious starting 2 days before they develop symptoms, or 2 days before the date of their positive test if they do not have symptoms.
- Get tested again 5-7 days after the end of isolation for the person with COVID-19.
- Wear a mask when in contact with the person with COVID-19 throughout the infected person’s isolation period.
- Wear a mask indoors in public until 14 days after the infected person’s isolation period ends or until the fully vaccinated close contact receives their final test result.
- Isolate immediately if they develop symptoms of COVID-19 or test positive.
What should I do if multiple people I live with test positive for COVID-19 at different times?
Recommendations for this situation depend on vaccination status:
- When multiple members of the household become infected at different times and the people with COVID-19 can’t isolate from other members of the household, close contacts who are unvaccinated or not fully vaccinated should
- Quarantine throughout the isolation period of any infected person in the household.
- Continue to quarantine until 14 days after the end of isolation date for the most recently infected member of the household. For example, if the last day of isolation of the person most recently infected with COVID-19 was June 30, the new 14-day quarantine period starts on July 1.
- Get tested 5-7 days after the end of isolation for the most recently infected member of the household.
- Wear a mask when in contact with any person with COVID-19 while that person is in isolation.
- Wear a mask when in contact with other people in the home until quarantine ends.
- Isolate immediately if they develop symptoms of COVID-19 or test positive.
- When multiple members of the household become infected at different times and the people with COVID-19 can’t isolate from other members of the household, close contacts who are fully vaccinated in this situation should
- Get tested 5-7 days after their first exposure. A person with COVID-19 is considered infectious starting 2 days before they developed symptoms, or 2 days before the date of their positive test if they do not have symptoms.
- Get tested again 5-7 days after the end of isolation for the most recently infected member of the household.
- Wear a mask when in contact with any person with COVID-19 while that person is in isolation.
- Wear a mask indoors in public until 14 days after the end of isolation for the most recently infected member of the household or until the fully vaccinated close contact receives their final test result. For example, if the last day of isolation for the person most recently infected with COVID-19 was June 30, the new 14-day period to wear a mask indoors in public starts on July 1.
- Isolate immediately if they develop symptoms of COVID-19 or test positive.
I had COVID-19 and completed isolation. Do I have to quarantine or get tested if someone I live with gets COVID-19 shortly after I completed isolation?
No. If you recently completed isolation and someone in your household tests positive for the virus that causes COVID-19 shortly after the end of your isolation period, you do not have to quarantine or get tested as long as you do not develop new symptoms. Once all members of the household have completed isolation or quarantine, refer to the guidance below for new exposures to COVID-19.
- People who had COVID-19, recovered, and completed 10 days of isolation and then during the 90 days following the end of isolation come into close contact with someone with COVID-19 do not have to quarantine or get tested if they do not have symptoms. But they should
- Wear a mask indoors in public for 14 days after exposure.
- Monitor for COVID-19 symptoms and isolate immediately if symptoms develop.
- Consult with a healthcare provider for testing recommendations if new symptoms develop.
- If more than 90 days have passed since recovery from infection, people who had COVID-19 should follow recommendations for close contacts based on their vaccination status.

BC COVID-19 Self-Assessment Tool

If you need help or guidance in another language, please call 8‑1‑1 which provides translation services in 130 languages.
The Ministry of Health, in partnership with Thrive Health, created this self-assessment tool to provide up-to-date guidance and recommendations for testing and follow-up for COVID-19 that follows BCCDC guidance. You can complete this assessment for yourself or on behalf of someone else. We do not recommend this tool for children under 2 years old; please see your healthcare provider.
This guidance is not to be used to determine suitability to attend/return to work or school.
This self-assessment tool is intended for COVID-19 only and does not replace your health care provider’s advice. Your symptoms may not be related to COVID-19 and could require you to seek medical attention.
If you have any concerns, feel very sick, or your symptoms are not improving, contact your family doctor/nurse practitioner or call 8-1-1.
COVID-19 and Children
Children generally have milder symptoms of COVID-19 than adults. Children may also present symptoms of COVID-19 differently than adults. For example, symptoms in children may be a change in activity level, appetite, or behaviour. For children, it’s important to think about what is usual or unusual about their specific symptoms. For more information visit COVID-19 and children .
Last updated: 07/19/2021 3:00 pm PDT
How to Protect Yourself & Others
Some people in your family need to continue to take steps to protect themselves from COVID-19, including
- Anyone not fully vaccinated, including children under 5 years of age who cannot be vaccinated yet
- People with weakened immune systems or underlying medical conditions

Get Vaccinated
- Authorized COVID-19 vaccines can help protect you from COVID-19.
- You should get a COVID-19 vaccine as soon as you can.
- Once you are fully vaccinated, you may be able to start doing some things that you had stopped doing because of the pandemic.
Wear a mask
- Everyone 2 years of age or older who is not fully vaccinated should wear a mask in indoor public places.
- In general, you do not need to wear a mask in outdoor settings.
- In areas with high numbers of COVID-19 cases, consider wearing a mask in crowded outdoor settings and for activities with close contact with others who are not fully vaccinated.
- People who have a condition or are taking medications that weaken their immune system may not be fully protected even if they are fully vaccinated. They should continue to take all precautions recommended for unvaccinated people, including wearing a well-fitted mask, until advised otherwise by their healthcare provider.
- If you are fully vaccinated, to maximize protection from the Delta variant and prevent possibly spreading it to others, wear a mask indoors in public if you are in an area of substantial or high transmission.
- If you are fully vaccinated, see When You’ve Been Fully Vaccinated.
Wearing a mask over your nose and mouth is required on planes, buses, trains, and other forms of public transportation traveling into, within, or out of the United States and while indoors at U.S. transportation hubs such as airports and stations. Travelers are not required to wear a mask in outdoor areas of a conveyance (like on open deck areas of a ferry or the uncovered top deck of a bus).
Stay 6 feet away from others
- Inside your home: Avoid close contact with people who are sick.
- If possible, maintain 6 feet between the person who is sick and other household members.
- Outside your home: Put 6 feet of distance between yourself and people who don’t live in your household.
- Remember that some people without symptoms may be able to spread virus.
- Stay at least 6 feet (about 2 arm lengths) from other people.
- Keeping distance from others is especially important for people who are at higher risk of getting very sick.
Avoid crowds and poorly ventilated spaces
- Being in crowds like in restaurants, bars, fitness centers, or movie theaters puts you at higher risk for COVID-19.
- Avoid indoor spaces that do not offer fresh air from the outdoors as much as possible.
- If indoors, bring in fresh air by opening windows and doors, if possible.
Wash your hands often
- Wash your hands often with soap and water for at least 20 seconds especially after you have been in a public place, or after blowing your nose, coughing, or sneezing.
- It’s especially important to wash:
- Before eating or preparing food
- Before touching your face
- After using the restroom
- After leaving a public place
- After blowing your nose, coughing, or sneezing
- After handling your mask
- After changing a diaper
- After caring for someone sick
- After touching animals or pets
- If soap and water are not readily available, use a hand sanitizer that contains at least 60% alcohol. Cover all surfaces of your hands and rub them together until they feel dry.
- Avoid touching your eyes, nose, and mouth with unwashed hands.
Cover coughs and sneezes
- If you are wearing a mask: You can cough or sneeze into your mask. Put on a new, clean mask as soon as possible and wash your hands.
- If you are not wearing a mask:
- Always cover your mouth and nose with a tissue when you cough or sneeze, or use the inside of your elbow and do not spit.
- Throw used tissues in the trash.
- Immediately wash your hands with soap and water for at least 20 seconds. If soap and water are not readily available, clean your hands with a hand sanitizer that contains at least 60% alcohol.
Clean and disinfect
- Clean high touch surfaces daily. This includes tables, doorknobs, light switches, countertops, handles, desks, phones, keyboards, toilets, faucets, and sinks.
- If someone is sick or has tested positive for COVID-19, disinfect frequently touched surfaces. Use a household disinfectant product from EPA’s List N: Disinfectants for Coronavirus (COVID-19)external icon according to manufacturer’s labeled directions.
- If surfaces are dirty, clean them using detergent or soap and water prior to disinfection.
Monitor your health daily
- Be alert for symptoms. Watch for fever, cough, shortness of breath, or other symptoms of COVID-19.
- Especially important if you are running essential errands, going into the office or workplace, and in settings where it may be difficult to keep a physical distance of 6 feet.
- Take your temperature if symptoms develop.
- Don’t take your temperature within 30 minutes of exercising or after taking medications that could lower your temperature, like acetaminophen.
- Follow CDC guidance if symptoms develop.
Links you should have handy
https://www.who.int/health-topics/coronavirus